inputtime:2022-08-02 10:42:37 From:Qilu Hospital
Recently, Professor Li Gang’s team from the Department of Neurosurgery, Qilu Hospital of Shandong University published a paper in an international prestigious magazine “Journal of Experimental & Clinical Cancer Research”, entitled “PDIA3P1promotes Temozolomide resistance in glioblastoma by inhibiting C/EBPβ degradation to facilitate proneural-to-mesenchymal transition”(Chinese Academy of Sciences (CAS) Journal ranking Q1, IF:12.658). The paper is the first to reveal a novel mechanism by which PDIA3P1 promotes drug resistance in glioblastoma. Professor Li Gang and attending doctor Zhang Ping of Qilu Hospital of Shandong University are joint corresponding authors. Gao Zijie, a postgraduate student of Qilu Hospital majoring in neurosurgery, is the first author of the paper.

Glioblastoma (GBM) is the most common malignant tumor in central nervous system, and the prognosis is extremely poor. Even after standard surgery, postoperative radiotherapy and chemotherapy and other comprehensive treatments, the median survival time is 15 months at most. The main reason why GBM is difficult to cure is not only that the tumor is difficult to remove, but closely related to the chemotherapy resistance of the tumor.
Temozolomide (TMZ) is the most widely used chemotherapy drug for GBM patients, but almost all patients who receive TMZ after surgery will experience recurrence after 7-10 months of progression-free survival. The heterogeneity and plasticity of cells in GBM are deemed to be the key factors driving treatment resistance and tumor recurrence. Based on the heterogeneity research of tumor gene expression profiles, there are at least three subtypes of GBM, i.e. pre-neuronal (Proneural, PN), classical (Classical, CL), and mesenchymal (Mesenchymal, MES). Compared with PN subtype patients with good prognosis and sensitive to radiotherapy and chemotherapy, GBM patients of MES subtype showed poor prognosis and strong resistance to radiotherapy and chemotherapy. Previous studies have shown that with the progress of the disease and tumor recurrence, the phenotype of GBM changes from PN type to MES type (Proneural-Mesenchymal Transition, PMT). PMT has also been recognized as a marker of tumor acquisition of multiple therapy resistance and recurrence.
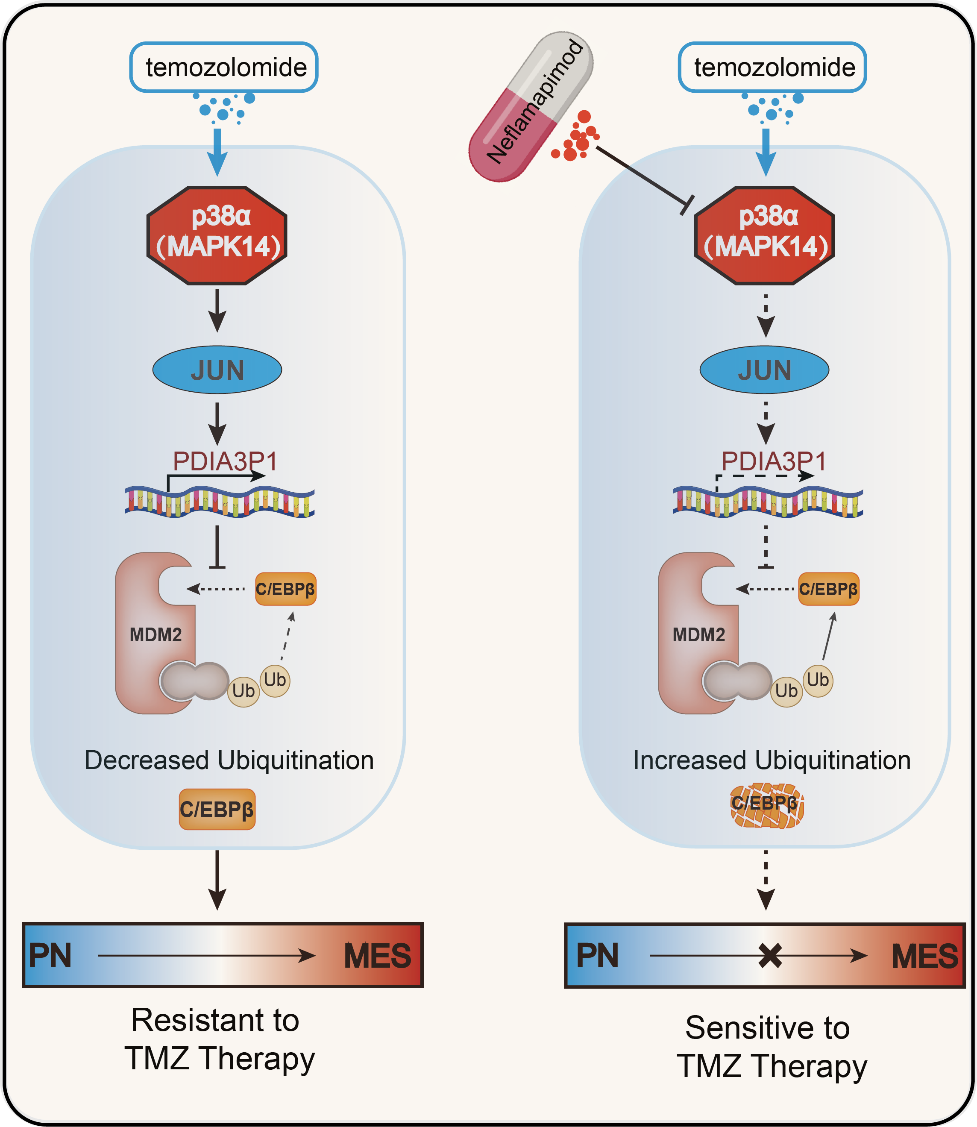
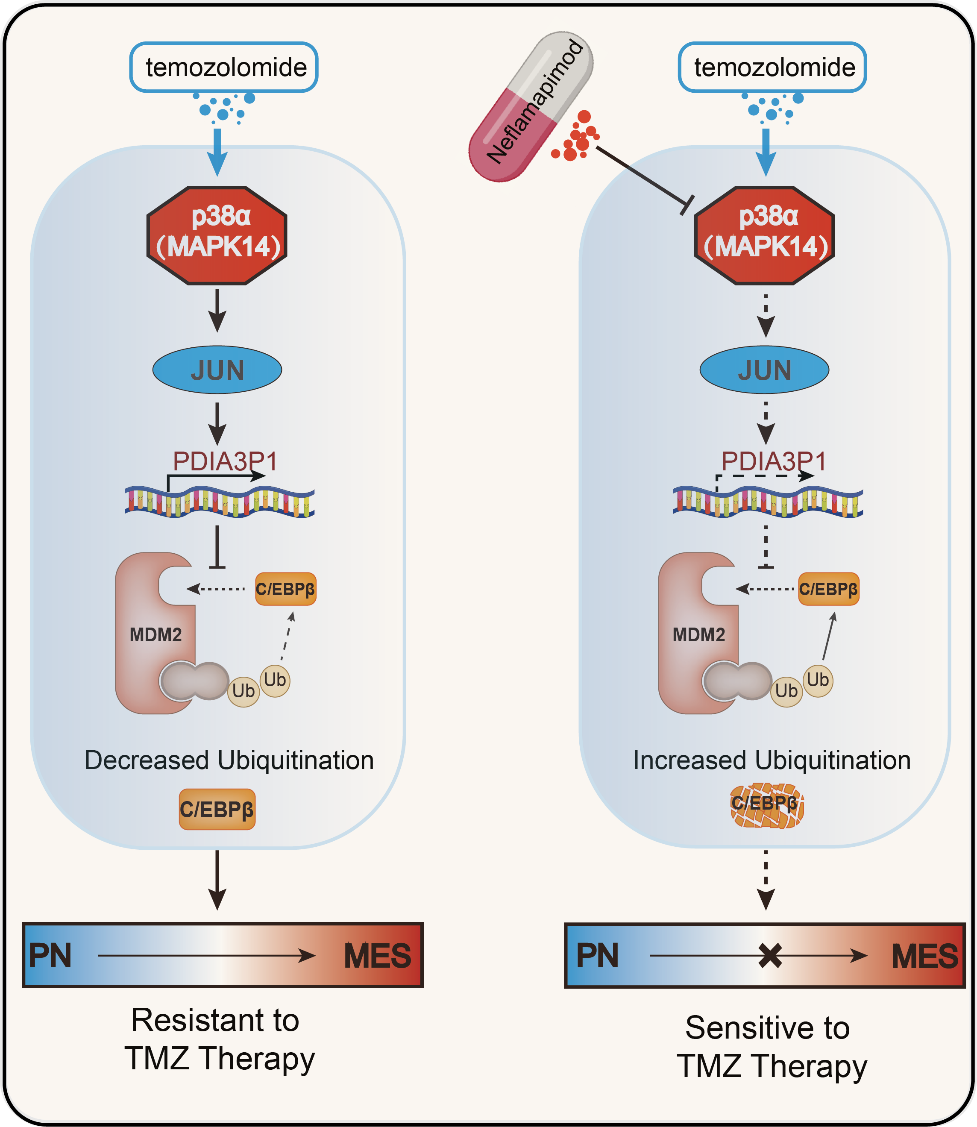
This study is the first to confirm that the pseudogene PDIA3P1 is highly expressed in drug-resistant glioma cells, and it confirmed that PDIA3P1 can promote the development of TMZ resistance in glioblastoma. In terms of the development mechanism, the researchers found that TMZ treatment can up-regulate the expression of PDIA3P1 through the p38α-MAPK signaling pathway, and PDIA3P1 promotes PMT by stabilizing the downstream molecule C/EBPβ, thereby making glioblastoma more resistant to chemotherapy. Through screening, it was found that Nefllamapimod, a targeted medicine, can inhibit the stress up-regulation of PDIA3P1, and the combination of Nefllamapimod and TMZ can exert a stronger anti-tumor effect.
Professor Li Gang's team has long been devoted to the research on the regulation of glioma immune microenvironment, phenotype transformation of glioma stem cells, and tumor chemoradiotherapy tolerance, etc. The research results were published in international prestigious journals including Mol Cancer, Adv Science, Mol Therapy, Oncogene, Cell Death Dis. This research is funded by National Natural Science Foundation of China and Mount Tai Scholars Climbing Program.
By Sun Yingtao, Chen Teng